<< Back
Why Deep Brain Stimulation ‘Life-Altering’ for Some Parkinson’s Patients
February 13, 2020
By Sarah Zurek, RN, BSN
Chase Family Movement Disorders Center
When it comes to Parkinson’s disease, essential tremor and dystonia, there is no cure but there are ways to reduce symptoms and improve your movement and quality of life.
One way is through the surgical procedure called deep brain stimulation (DBS).
“It can be a life-altering procedure for patients,” said Dr. Patrick Senatus, medical director of the Deep Brain Stimulation Program at the Ayer Neuroscience Institute Chase Family Movement Disorders Center.
The multidisciplinary providers conduct a comprehensive evaluation to determine if DBS is the right treatment option for you. This includes a functional assessment of your symptoms, neuropsychological testing and a neurosurgical evaluation.
Q. How does DBS work?
A. DBS uses electrical impulses to stimulate a targeted area in the brain and affect movement by altering activity there. Unlike other surgical procedures for treating movement disorders, DBS does not destroy brain tissue, stimulation is adjustable and the procedure is reversible.
Typically, two separate surgical procedures are required to receive DBS therapy. The first is to implant a thin wire (lead) into a specific, predetermined area of the brain.
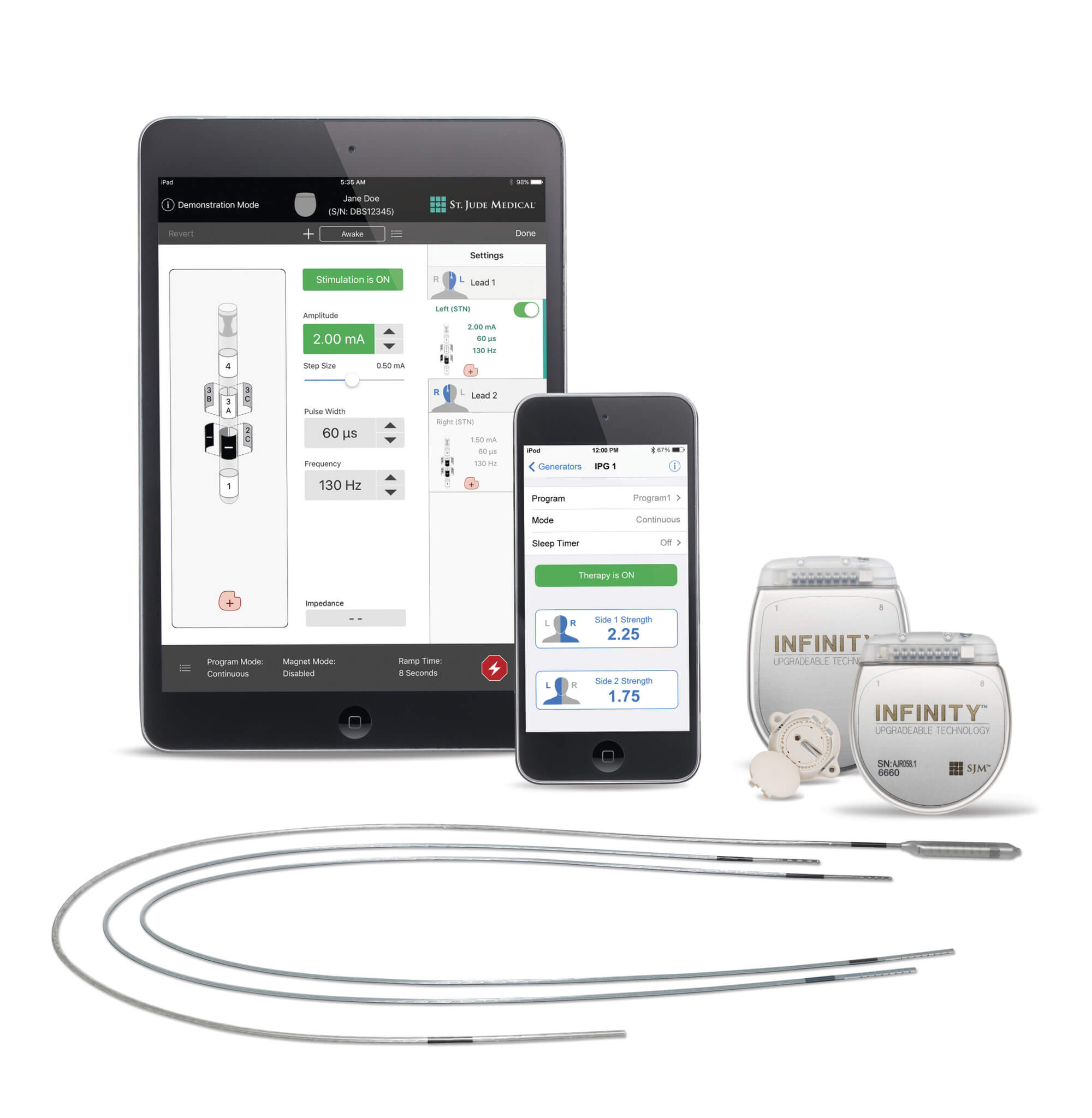
The second, a few weeks later, is to implant a small, battery-powered device (pulse generator) like a pacemaker in the chest and connect it using an extension to the electrodes in your brain. The entire system is implanted beneath the skin. (Above, the Abbott Deep Brain Stimulation System with app.)
About four weeks after the first surgery, the neurologist will start to program the generator during an office visit. It takes several programming sessions to deliver the best level of stimulation for relieving symptoms.
Q. What should I expect?
A. Before surgery, you will meet with members of the DBS team. You can expect neurological and neurosurgical exams, neuropsychological testing, lab tests and an MRI. Together, you and the team will decide whether to go forward with the procedure or not.
If you opt for surgery, we will help you prepare by giving you pre-operative instructions and answering any additional questions. For the first surgery, you can expect to stay one night in the hospital. The second surgery is an outpatient procedure and you will go home the same day. There are rechargeable and non-rechargeable generators available and you can decide with Dr. Senatus which would be best for you.
Q. After the procedure?
A. You will have check-ups at least every three months to assess your symptoms and make sure your generator is working properly.
The nonrechargeable pulse generator has a battery life of three to five years. Generally, the generator must be replaced when power is depleted. Rechargeable pulse generators can last 15 years before replacement is needed.
“The upper length of time that DBS can be effective hasn’t been determined,” Dr. Senatus said. “It can potentially last indefinitely.”
For more information on DBS for Parkinson’s, essential tremors and dystonia at the Hartford HealthCare Chase Family Movement Disorders Center, click here.