<< Back
How Far Away Is a Universal COVID-19 Vaccine for All Strains?
March 17, 2022
The breathtaking development of the COVID-19 vaccine took Moderna researchers using messenger RNA, or mRNA, technology only about 48 hours after receiving the coronavirus’ genome sequence in January 2020.
That was for the original strain. Creating a vaccine for subsequent strains, notably Delta and Omicron, or, even better, an all-purpose vaccine for all strains is proving a bit more traditional — when progress is measured in months or years instead of hours.
“What would really be wonderful,” says Dr. David Regelmann, Program Director for Internal Medicine at St. Vincent’s Medical Center in Bridgeport, “and I think the mRNA technology is there, would be to have a vaccine that’s more universal and longer-lasting.”
The federal government’s Operation Warp Speed accelerated clinical testing and manufacturing, bringing vaccines to the public in less than a year. (The Pfizer-BioNTech vaccine, which also uses mRNA technology, was the first COVID-19 vaccine authorized by the Food and Drug Administration. Its development was not funded by Operation Warp Speed.) Several Phase One studies on a universal vaccine have started, but it could take at least three years to reach a finished product.
At least seven known coronaviruses infect humans. Several hundred more infect animals. SARS-CoV-2, the virus that causes COVID-19, is the one scientists are hoping to wrangle. A coronavirus spike protein attaches to cells, then attacks them, which encourages the body’s immune system to produce antibodies that seek out these spike proteins and neutralize them. An mRNA vaccine essentially has the built-in code for the coronavirus’ spike protein. Once vaccinated, your body produces the spike protein that automatically triggers an immune response and protection against the actual virus.
Moderna is now working on a Omicron-specific vaccine and another version now in Phase Two trials that combines the original vaccine with an Omicron-specific candidate. Pfizer is also investigating an Omicron-specific vaccine and another pan-coronavirus vaccine that offers protection against several variants.
The National Institute of Allergy and Infectious Diseases has awarded millions in funding to academic researchers, included those at Harvard Medical School’s Brigham and Women’s Hospital, Duke University and the University of Wisconsin.
Affinivax and VBI Vaccines, each with headquarters in Cambridge, Mass., are developing vaccines with spike proteins from several coronaviruses on a single particle.
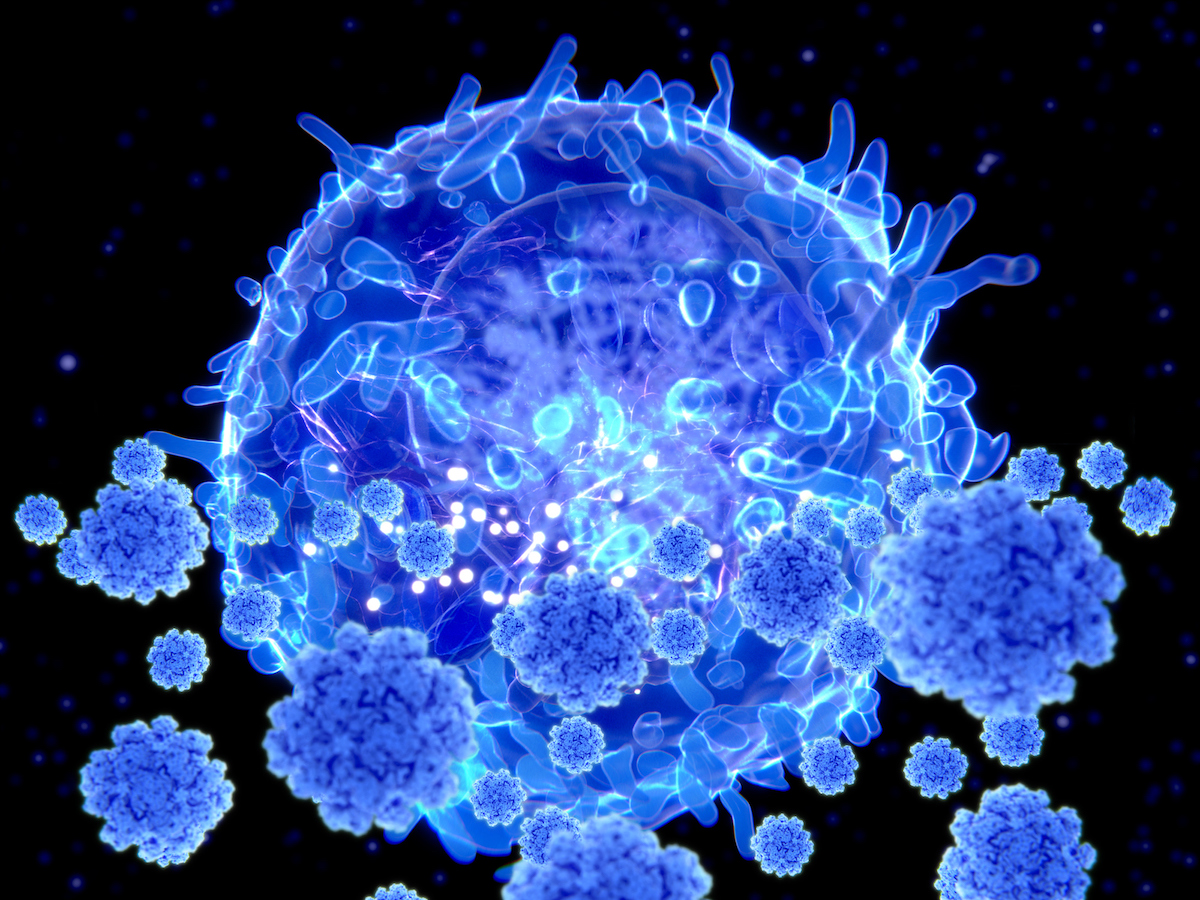
The spike protein is the foundation of current COVID-19 vaccines, but researchers are also interested in T cells (see photo above) that target the entire SARS-CoV-2 virus. Codiak Biosciences, another Cambridge biotech company, is also working on a vaccine that guide T cells to eliminate infected cells from the body, limiting the severity of an infection by the actual virus.
For now, Pfizer has asked the FDA to approve the emergency use of a second booster for people at least 65 years old, citing data from two Israel studies that still await peer review.
“With a second booster, or fourth dose, of an mRNA vaccine,” says Dr. Regelmann, “they were seeing about a fourfold decrease in severe illness from COVID-19 and hospitalizations.”